Abstract
Introduction: Allogeneic hematopoietic cell transplant for acute myeloid leukemia (AML) is curative for a subset of patients, however carries a substantial risk of adverse outcomes. The American Society for Blood and Marrow Transplant (ASBMT) and European Leukemia Network (ELN) each provide distinct algorithms for predicting likelihood of leukemia-free survival after transplant that differ from one another, although the former is used as a means of comparing success among different institutions. The current study represents a single-center, retrospective analysis of a more homogeneous patient population with the goal of comparing the predictive value of the ASBMT vs. ELN risk stratifications for relapse after allo transplant.
Methods: Data were obtained from the transplant registry of the UCLA Hematological Malignancies/Stem Cell Transplant program and from electronic medical records of patients undergoing allogeneic transplant for a diagnosis of AML in remission between January 2008 and September 2015. Fischer's exact (categorical variables) were used to determine differences between relapsed and non-relapsed patients, while Cox proportional-hazards regression was used to determine how time-to-relapse varied for ASBMT risk categories and ELN risk (high vs. intermediate or low) with statistical software (SAS v. 9.4). For the time-to-relapse analyses, patients not relapsing by the last UCLA clinic visit were included as censored patients, while patients who died prior to relapse were treated as a competing risk.
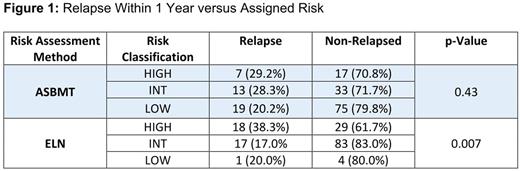
Results: 169 adult patients undergoing allogeneic transplant for AML were included in the analysis; 49 pts relapsed by June 2016. Median time-to-relapse was 158 days (range: 41-2449) and for non-relapsed pts median follow-up was 547 days (range: 31 - 2893). Median age for relapsed pts was 54 years (range: 21-71) and for non-relapsed pts was 55 years (range: 18- 75). 5 patients were excluded from analysis due to relapse within 30 days, and another 12 patients were missing cytogenetic or molecular information and were not included in the ELN risk analysis (17 total). 24 subjects were categorized by ASBMT as high-, 46 intermediate-, and 94 low-risk. According to ELN categories, 47 subjects were considered high-, 100- intermediate-, and 5 low-risk. Median time-to-relapse was 258 (range: 35-2100) days in ASBMT high-risk patients as compared to 395 days (range: 2-2893) in ASBMT intermediate- or low-risk groups whereas time-to-relapse was 214 days (range: 2-2429) for ELN high-risk patients vs. 496.5 (range: 20-2893) days in the intermediate/low groups. For ASBMT high-risk disease patients, there were no statistically significant differences in relapse rate and time-to-relapse when compared to intermediate-/low-risk patients (p=1.0), but when using ELN criteria, high-risk disease was more likely to be identified among relapsed patients (p=0.036). For patients who relapsed within 1 year compared to those who remained in remission at 1 year, ASBMT risk categories were not significantly different among those who relapsed and those who did not (p=0.6) but ELN high-risk disease was identified more frequently among patients who relapsed rather than those who did not (p=0.012). While no significant differences in time-to-relapse were seen for ASBMT high-risk disease vs. intermediate-/low-risk disease patients (1.17 (0.51-2.70); p=0.72),time-to-relapse was significantly decreased by the presence of ELN high-risk disease [0.49 (0.27-0.87); p=0.016] [hazard ratio (95% confidence interval); p-value]. Of the 152 patients analyzed for relapse, 47 were ELN high-risk, of which 42 (89%) were mis-categorized as ASBMT intermediate- or low-risk.
Conclusions: While no differences were found among ASMBT risk stratification groups in our database, the presence of ELN high-risk disease was found to significantly increase the risk of relapse after allogeneic stem cell transplant compared to lower-risk disease patients. Our data confirm findings of Quek et al. that further corroborate the value of assessing AML mutational status, discovering an increased propensity of relapse depending on known AML mutations, something considered only in the ELN assessment tool but not in the ASBMT criteria (Quek et al, Blood 2016). The improved predictive value of the ELN criteria is validation of the importance of molecular and cytogenetic information in characterizing AML disease behavior.
Schiller: bluebird bio: Research Funding; mateon therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal